Macular Degeneration
Macular degeneration is a deterioration or breakdown of the macula. The macula is a small area in the retina at the back of the eye that allows you to see clearly. When the macula is not functioning correctly, your central vision can be affected by blurriness, distortion or dark areas. Macular degeneration is the leading cause of severe vision loss in the United States in people 65 years or older.

Many older people develop macular degeneration as part of the body's natural aging process. The most common form of macular degeneration is age-related macular degeneration (AMD). There are two common types of AMD.
Most people (about 90%) have a form of AMD called "atrophic" or "dry" AMD, which develops when the tissues of the macula grow thin with age. Dry AMD usually causes a slow loss of vision.
A second smaller group of people (about 10%) have a more serious condition called "exudative" or "wet" AMD. Wet AMD occurs when abnormal blood vessels grow underneath the retina. These unhealthy vessels leak blood and fluid, which can scar the macula. For patients with wet AMD, vision loss may be rapid and severe.
Some symptoms of macular degeneration may be:
- A dark or empty area appears in the center of vision
- Blurred vision
- Distortion of lines and shapes
Dry AMD cannot be treated with medication or surgery, but many patients can function well with magnifying lenses. Treatment for wet AMD can include one or a combination of the following:
- Thermal Laser
- Photodynamic Therapy (PDT)
- Anti-VEGF Injections
Diabetic Retinopathy
If you have Diabetes your body does not utilize sugar properly, and when sugar levels rise, damage to the blood vessels in the retina may occur. This damage is known as diabetic retinopathy and is currently a leading cause of blindness in adults in the United States.

There are two types of diabetic retinopathy:
Non-Proliferative (Background) Diabetic Retinopathy is the early stage where small retinal blood vessels break and leak
Proliferative Diabetic Retinopathy is when new blood vessels grow abnormally within the retina (neovascularization). This new growth can cause vitreous hemorrhage, scarring or retinal detachment, which can lead to vision loss.
Symptoms of diabetic retinopathy and its complications may include:
- Blurred or distorted vision or difficulty reading
- Floaters
- Partial or total loss of vision or a shadow or veil across field of vision
Retinal Vascular Disease
Blood vessels carry blood to and from the light sensitive structure in the back of the eye called the retina. Blood from the retina is drained from smaller branches of retinal veins into the larger central retinal vein and away from the eye. A retinal vein occlusion occurs when one of these veins is blocked or obstructed. Symptoms of retinal vascular disease are sudden blurring or loss of vision in all or part of one eye.
There are two different types of retinal vein occlusion. Central retinal vein occlusion (CRVO) occurs when the main vein of the eye becomes blocked. Branch retinal vein occlusion (BRVO) occurs when one of the smaller branches of vessels becomes blocked.
Certain illnesses increase your risk for developing retinal vein occlusion including:
- Diabetes
- Glaucoma
- High blood pressure
- Cardiovascular disease
Complications of retinal vein occlusion may include:
- Macular edema or swelling of the macula which causes blurred and/or decreased vision
- Abnormal blood vessel growth or neovascularization.
- Neovascular glaucoma or painful pressure in the eye can occur in severe cases of CRVO
There is no known cure for retinal vein occlusion though the complications listed above can be treated with intravitreal injections or laser surgery to stabilize or improve vision. You may be able to prevent retinal vein occlusion from occurring by properly managing any health conditions which increase the risk of retinal vascular disease.
Floaters and Flashes
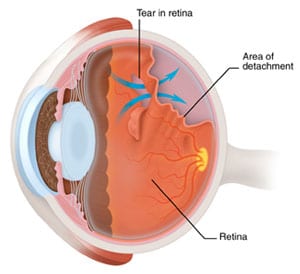
Floaters appear as small specks or clouds moving in your field of vision. You may see them more clearly when looking at a plain background, such as a blank wall. Floaters are actually tiny clumps of gel or cells inside the vitreous, the clear jelly-like fluid that fills the inside of the eye. Floaters can have different shapes such as little dots, circles, lines, clouds or cobwebs. Floaters may be a symptom of a tear in the retina, which is a serious problem because it may lead to retinal detachment. Other floaters are harmless and fade over time, requiring no treatment.
When people reach middle age, the vitreous gel may start to thicken or shrink, forming clumps or strands inside the eye. Floaters often occur when the vitreous gel pulls away from the back wall of the eye, causing a posterior vitreous detachment. In some cases the retina can tear if the shrinking vitreous gel pulls away from the wall of the eye.
When the vitreous gel inside your eye rubs or pulls on the retina, you may see what looks like flashing lights or lightning streaks. These flashes of light can appear off and on for several weeks or months. As we grow older, it is more common to experience flashes.
You should see your ophthalmologist as soon as possible if:
- One new, large floater or "showers" of floaters appear suddenly.
- You see sudden flashes of light.
Retinal Detachment
A retinal detachment occurs when the retina is pulled away from its normal position. A retinal detachment is a medical emergency which if not promptly treated, can cause permanent vision loss or blindness. Fortunately, retinal detachment has clear warning signs and symptoms including:
- Flashing lights
- New floaters
- A shadow or curtain over a portion of your field of vision
- Sudden blurred vision
These symptoms do not always mean a retinal detachment is present; however, you should see your ophthalmologist as soon as possible.
Unfortunately, many people don't appreciate the urgency of the warning signs of retinal detachment and they tend to put off seeing a doctor in the hope that symptoms will disappear. In some cases, symptoms temporarily diminish only to be followed by a loss of vision over the next few days or weeks caused by advanced retinal detachment. At this stage, retinal detachment can't always be successfully repaired and vision loss may be permanent. It is crucial to see your ophthalmologist at the earliest signs of retinal detachment.
Surgery is the only effective treatment for retinal detachment. The decision about which type of surgery and anesthesia to use depends upon the characteristics of your detachment.
If you are interested in learning more about any of these conditions or our services and procedures, call 718-575-8434 today to schedule an appointment.